Effective Revenue Cycle Management (RCM) is essential to maintaining the financial health of hospitals and healthcare systems. In 2025, as government-driven Medicare budget cuts loom, refining RCM processes is no longer optional—it’s critical. Healthcare organizations must enhance billing accuracy, streamline claims processing, strengthen denial management, and ensure compliance, all while prioritizing the patient experience.
Globally, healthcare systems lose approximately $125 billion each year due to RCM inefficiencies. At Pena4, our human-led expertise delivers actionable strategies to boost RCM performance. In this blog, we explore 10 keyways to elevate your hospital’s revenue cycle through precision, efficiency, and patient-focused solutions.
Note: This blog reflects on the improvements that healthcare partners can take to rectify their top RCM mistakes in 2025.
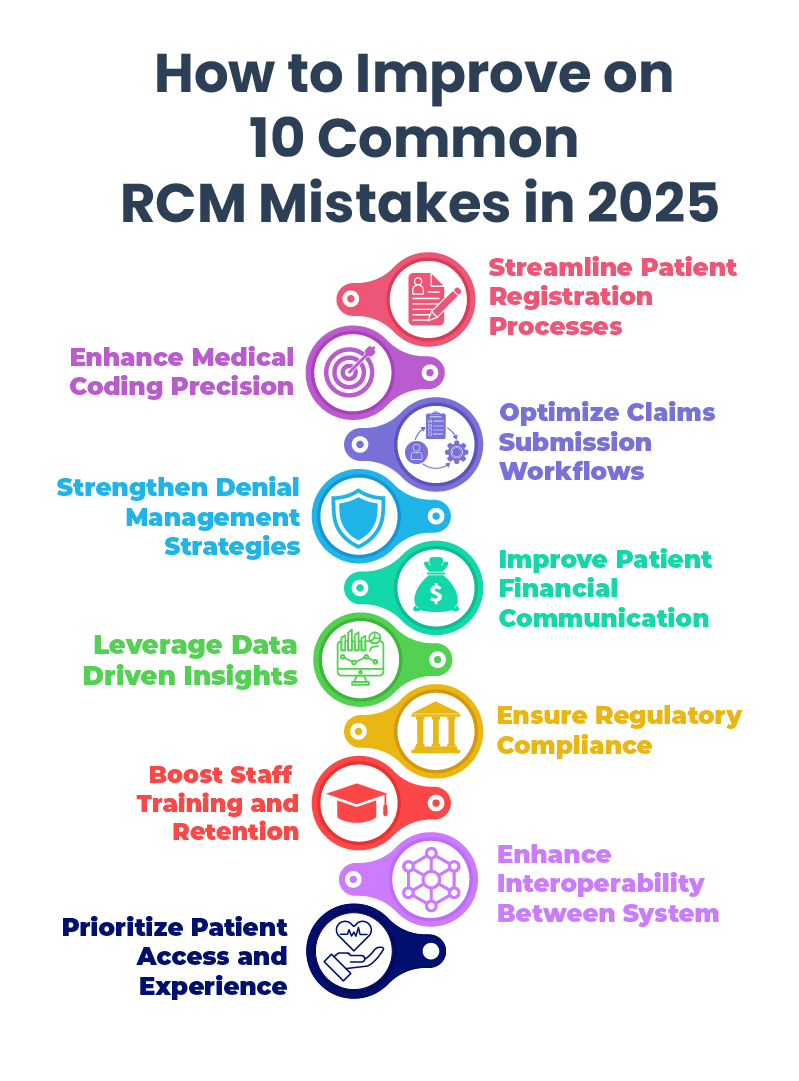
1. Streamline Patient Registration Processes
Accurate patient registration is the cornerstone of a healthy revenue cycle. Standardize intake protocols to ensure complete and verified patient information from the start. Real-time insurance eligibility checks can significantly reduce downstream claim denials.
Up to 46% of claim denials are caused by registration errors. Pena4 can help your team implement accurate, consistent front-end processes.
2. Enhance Medical Coding Precision
Correct medical coding is essential for proper reimbursement. With more than 420 new ICD-10, CPT, and HCPCS code updates expected in 2025, ongoing education and regular audits are a must.
Coding errors account for 77% of global claim denials. Pena4’s certified coders and provide expert guidance and support for maximum accuracy and compliance.
3. Optimize Claim Submission Workflows
Delays in claim submission interrupt cash flow. Implement multidisciplinary oversight teams to review unbilled accounts and conduct pre-bill checks, ensuring clean, timely claims.
Well-designed workflows can reduce rejections, especially with Pena4’s RCM Experts.. Pena4 creates tailored solutions to increase claim acceptance rates and reduce processing time.
4. Strengthen Denial Management Strategies
Proactive denial management is key to recovering lost revenue. Analyze denial trends, identify root causes, and apply corrective actions quickly.
Most of denied claims are recoverable. Pena4 helps you build strong denial prevention and recovery strategies.
5. Improve Patient Financial Communication
Transparent, compassionate communication enhances both collections and patient satisfaction. Offer pre-service cost discussions and flexible payment options.
Clear communication can increase patient payments. Pena4’s Patient Access Experts train staff to handle financial conversations with empathy and clarity.
6. Leverage Data-Driven Insights
Use real-time analytics to identify performance gaps and optimize operations. Monitor KPIs such as denial rates, clean claim ratios, and Days Sales Outstanding (DSO).
Organizations use analytics reports to increase revenue capture. Pena4’s data specialists help translate insights into results.
7. Ensure Regulatory Compliance
Keeping up with evolving regulations like HIPAA, CMS rules, and the No Surprises Act is non-negotiable. Regular training and audits are essential for avoiding costly fines.
Non-compliance costs the healthcare industry $6.9 billion annually. Pena4’s compliance team offers proactive, customized solutions to stay audit ready.
8. Boost Staff Training and Retention
An experienced, well-trained RCM workforce is your strongest asset. Offer continuous professional development and create a culture of retention.
High staff turnover can cost hospitals $5.8 million annually. Pena4’s workforce solutions focus on long-term engagement and skill-building.
9. Enhance Interoperability Between Systems
Seamless integration between RCM platforms and EHR systems ensures accurate data transfer and reduces administrative burden.
Interoperability can boost billing efficiency exponentially. Pena4 specializes in breaking down data silos for a more connected revenue cycle.
10. Prioritize Patient Access and Experience
Digital tools like online scheduling, pre-visit verification, and mobile check-ins improve both the patient journey and operational efficiency.
An integrated intake process can increase patient satisfaction by 35%. Pena4 helps design access strategies that support both patients and providers.
Conclusion: Partner with Pena4 for RCM Excellence
In 2025, optimizing your hospital revenue cycle is vital for both financial performance and exceptional patient care. Pena4 brings deep human expertise across coding, compliance, and patient access to help healthcare organizations thrive in a changing landscape.
Whether you’re looking to reduce claim denials, improve billing accuracy, or enhance the patient’s financial experience, Pena4 delivers smart, scalable solutions tailored to your needs.
Contact us at www.pena4.com to elevate your Revenue Cycle Management today.