Still looking for something?
Would you like us to assist you in finding what you’re looking for?
Would you like us to assist you in finding what you’re looking for?

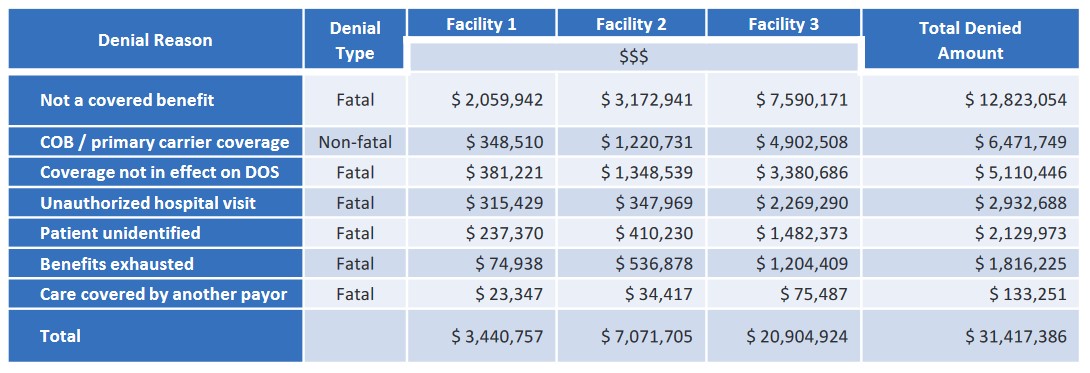
Hospital claims were denied for various patient access related issues. Client requested for a special project to perform root cause analysis, review claims, overturn denials and forecast cash opportunities.