Note: In this blog we will discuss in detail preventative strategies for denials in healthcare establishments.
To read about various steps involved in the denial management process
Read: All you need to know about Denial Management in 2025.
Introduction
In 2025, healthcare establishments across the United States are grappling with a confluence of formidable challenges. These include surging operational costs driven by inflation and pharmaceutical expenses, coupled with increasing demand for healthcare services. Simultaneously, providers face significant revenue-side pressures from escalating denial rates and the budgetary impact of the One Big Beautiful Bill Act (OBBBA), particularly affecting rural healthcare.
Given these financial headwinds, optimizing the denial management stage of the revenue cycle offers a critical opportunity for providers to curb losses and enhance revenue efficiency. A recent survey highlights the deteriorating relationship between providers and commercial payers, with 78% of hospitals reporting worsening experiences. Furthermore, 84% of respondents indicated a year-on-year increase in the cost of complying with insurer policies.
In light of these pressing concerns, we have compiled a comprehensive list of key denial management practices. Implementing these strategies can empower healthcare providers to effectively reduce revenue leakage, mitigate the financial burden of compliance, and significantly improve their clean claim submission rates.
Key Practices to Prevent Denials in Healthcare Establishment
Information Gathering
Tracking denied claims is essential to prevent significant revenue loss and mitigate administrative complexities. Without proper oversight, a rise in refused claims directly impacts an organization's financial health and operational efficiency.
Effective tracking can begin by gathering all the information with respect to denials from various payers. Additionally, information gathering for denials can also be sourced by Specialty, Location, and Provider.
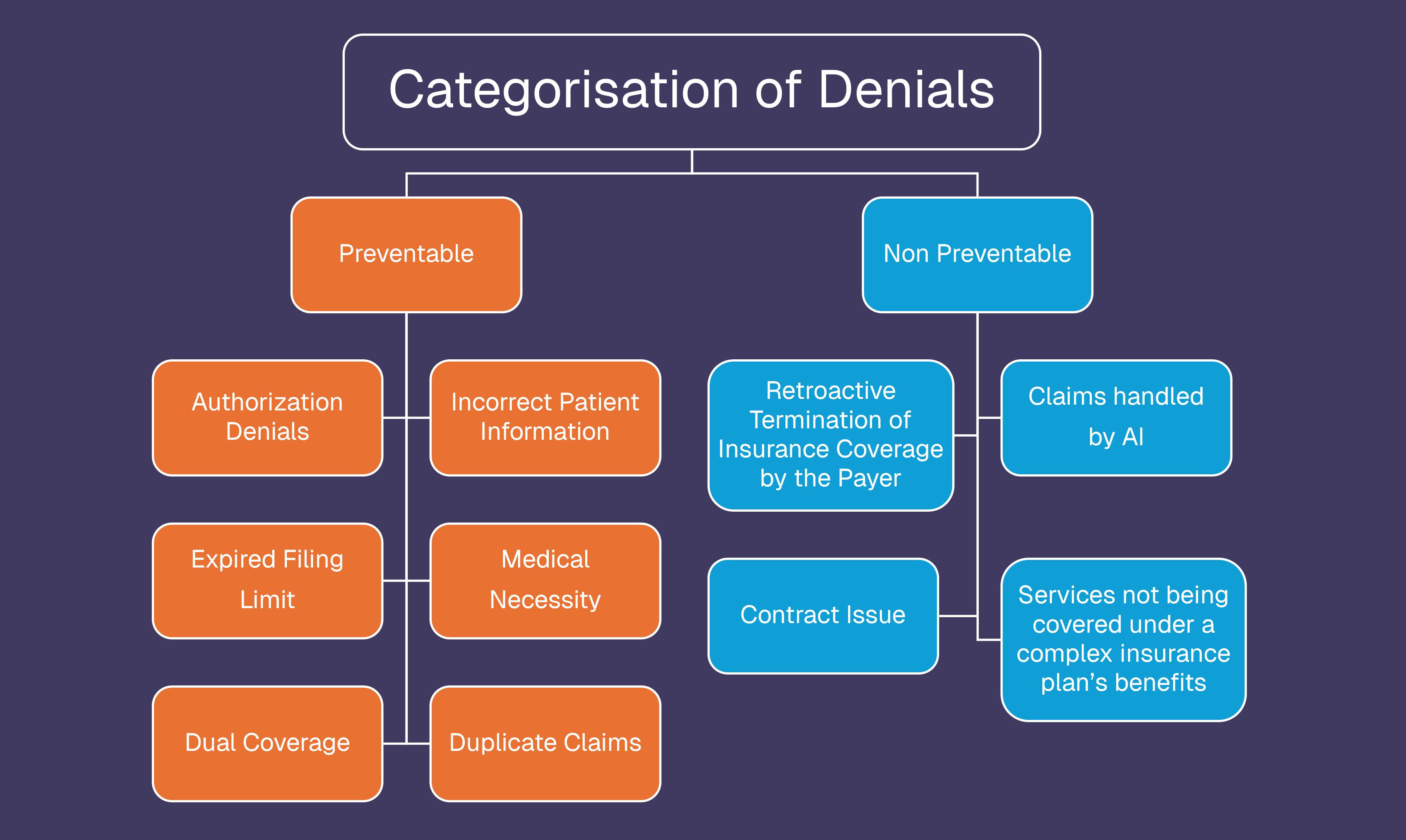
Categorization of Denials
This is an important step. In this step, the denial specialist must be able to categorize denials into many ways. Categorization of denials is as follows:
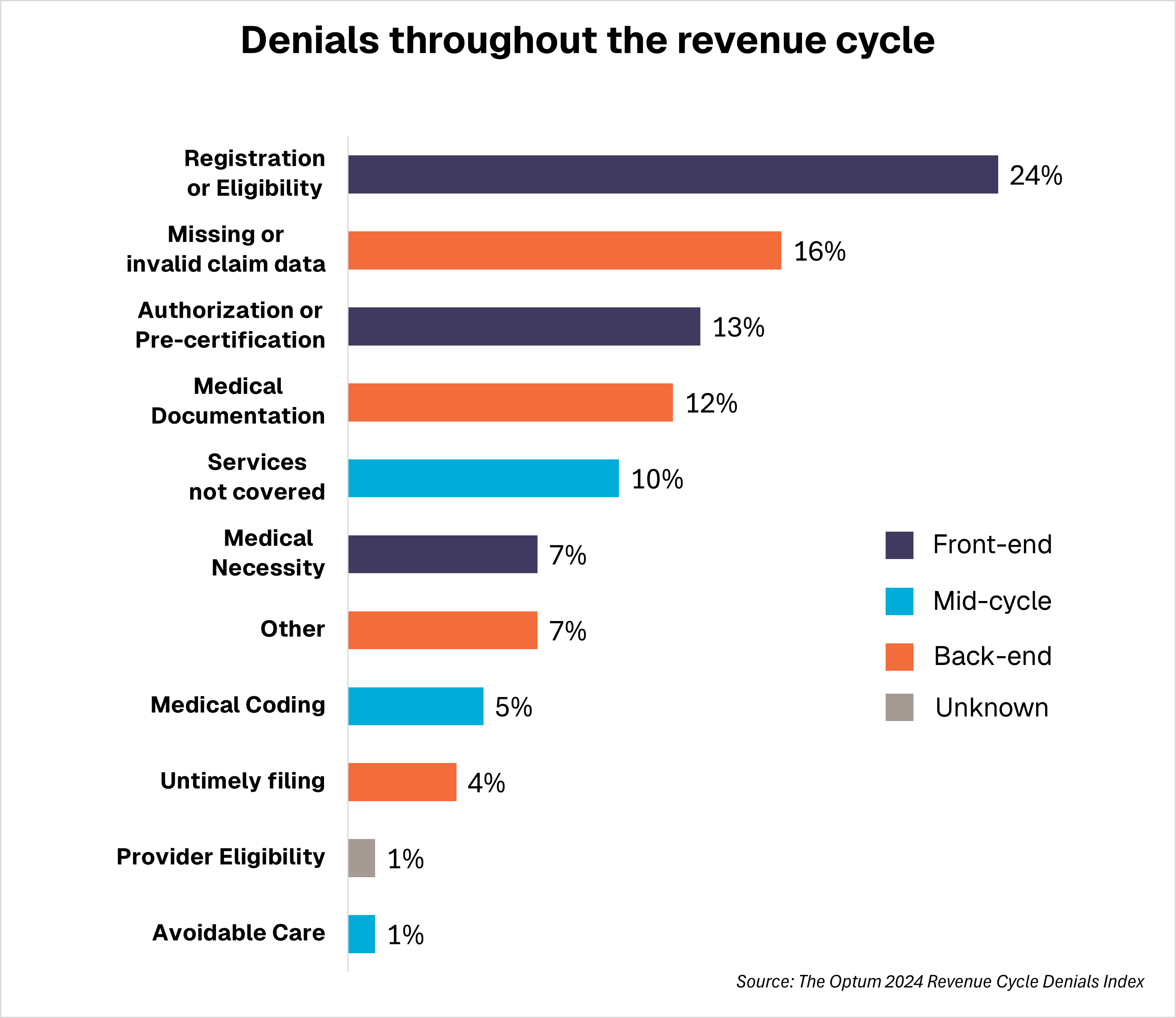
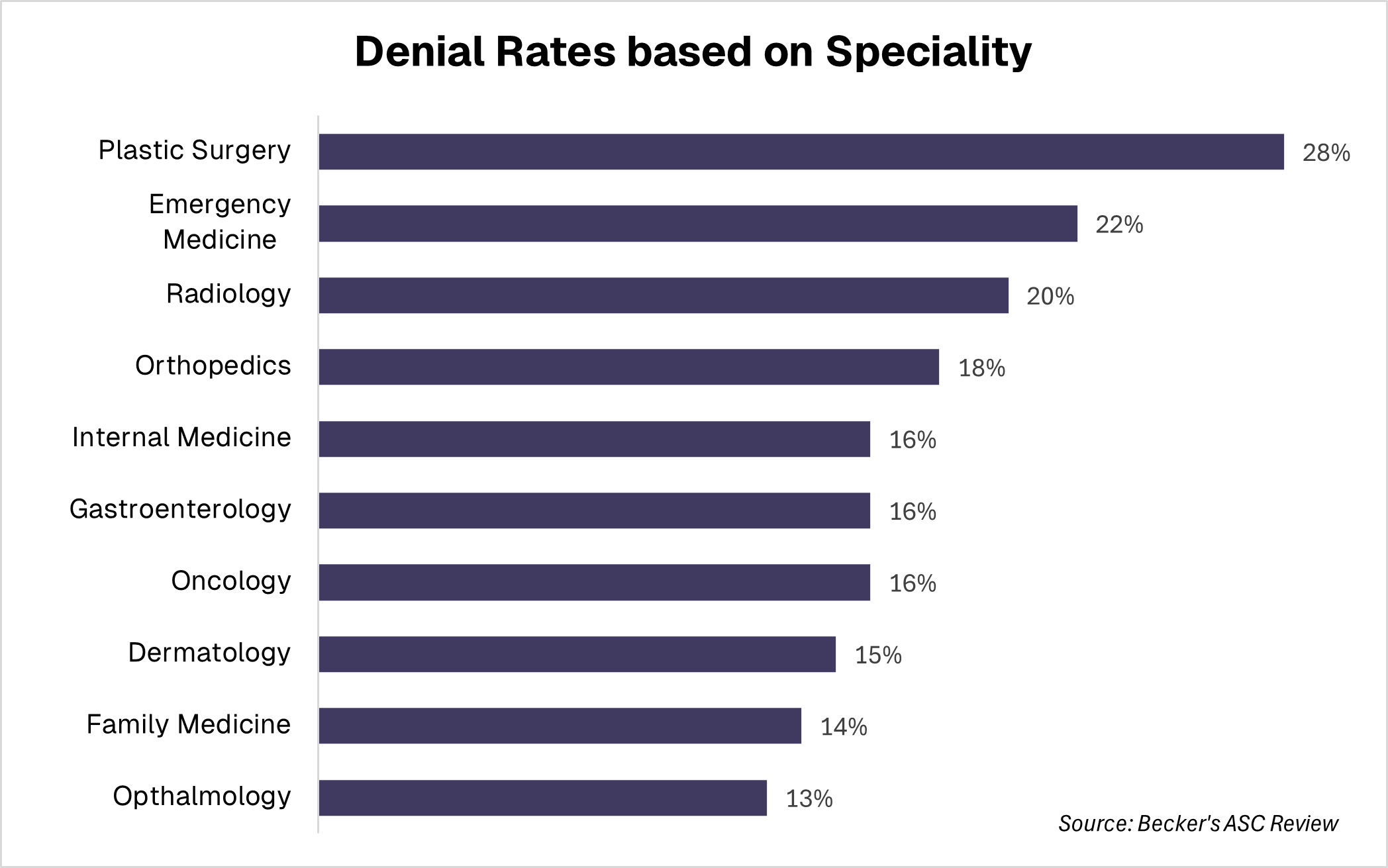
Identifying Denial Trends
Understanding the statistics and dissecting the root causes of denials is equally crucial for optimizing revenue. It is imperative to monitor denial trends comprehensively, not only based on each stage within the revenue cycle but also across different medical specialties. The graphs presented below illustrate denial rates in relation to various stages of the revenue cycle and by specific medical specialties.
Internal Process Improvement
Both small and large practices can significantly improve their denial rates by adhering to best practices such as staff training, maintaining clinical documentation integrity, coding diagnoses to the highest level of specificity, keeping billing software updated, and regularly reviewing payer policies.
For larger practices, it's important to go beyond the basics. They should set up a dedicated Denial Management Team, which includes leaders from coding, revenue cycle, and Health Information Management (HIM). This is especially useful when there are staff shortages or limited in-house expertise, which is a challenge for both small and large practices.
This team can implement a robust metric system to pinpoint the exact origin and reasons for denials, even identifying the individual employees involved.
Use of Digital Technology
With the advent of Electronic Health Records, evolution in Medical Practices’ operations is bound to happen. In this direction, organizations have to make significant investments to leverage capacities of software for denial management and appeals. This is especially true for practices facing staffing shortages or expertise deficits, regardless of their size.
Larger practices, in particular, can significantly benefit from upgrading their claims technology, embracing automation, and streamlining workflows. They can also enhance the patient experience by setting up patient portals and digitizing the onboarding process. Ensuring that coding software and claim scrubbing tools are effective against all payers, especially Medicare, is also vital. Ultimately, the strategic adoption of digital technology ensures critical Revenue Cycle Management (RCM) administrative tasks are also completed efficiently and on time.
At Pena4’s we use our in-built ‘Guru Auditor’, that helps us achieve coding accuracy and compliance with confidence. Guru Auditor is a web-based application that can be accessed anytime and anywhere, providing insightful performance reporting and streamlined audit management.
NEVER EVER miss payer deadlines
It might seem unbelievable, but providers frequently miss payer deadlines. This often stems from staff shortages, inexperienced employees, lack of awareness about specific deadlines, administrative errors, or incomplete documentation. Losing revenue due to missed deadlines poses a serious threat to an organization's financial health. To mitigate this, providers can consider outsourcing to experienced vendors like Pena4, who can scale services up or down based on your needs and keep track of all deadlines.
Focus on Quality over Quantity
To manage denials efficiently, organizations should focus their resources on claims that are easy to overturn, have readily available documents, match staff expertise, and where enough personnel are available.
As indicated by the above figure, automating the registration and eligibility stage is highly effective in preventing future denials. Concentrated efforts in this area can yield substantial long-term benefits. Similarly, the denial amount itself plays a crucial role in determining whether pursuing an appeal is financially viable.
Collaboration with Payers
A strong partnership between payers and providers benefits everyone. Providers receive timely reimbursements, while payers get the necessary documentation to verify coverage and service benefits. Additionally, practices short on staff can also use clearinghouse services, which explain denial reasons clearly and help resolve them faster.
Anticipating Future Denials Before Submission
A crucial element of a strong denial management strategy is anticipating future denials, particularly those that are unavoidable. This foresight allows organizations to proactively prepare by ensuring they have the necessary staff and expertise readily available. The goal is to resolve these denials as quickly and cost-effectively as possible.
Conclusion
With the 2025 Medicare budget cuts, healthcare practices especially in rural areas are already facing financial stress. That’s why denial management is now critical for survival. Following these best practices will: reduce revenue losses, improve the efficiency of the entire revenue cycle and support long-term stability of healthcare establishments.
Worried that you lack staff or expertise to implement above suggestions in your RCM? Don’t Worry! Pena4 has got you covered
Pena4’s medical billing solutions handle claim submission, charge entry, follow-ups, and denial management - improving reimbursements, fewer denials, and reduced administrative burdens for you. Let our experts simplify your billing process and maximize your revenue.